Vitamin D, often nicknamed the “sunshine vitamin”, is a vital nutrient that many of us do not get enough of. From supporting sturdy bones to bolstering our immune system, vitamin D plays diverse roles in keeping us healthy. In this comprehensive guide, we will explain exactly what vitamin D is, why it is important, how to spot a deficiency, and how to get enough through foods or supplements. We will also discuss the best supplements, safe dosage guidelines (including for children and during pregnancy), and what happens if you have too much or too little.
Whether you are wondering about the difference between vitamin D and D3, looking for foods high in vitamin D, or trying to figure out the best time to take your daily dose, we have got you covered. Let us shed some light on vitamin D and help you make sure you are getting the most from this essential sunshine nutrient.
What is vitamin D?
Vitamin D is a fat-soluble vitamin (not water-soluble) that functions more like a hormone in the body. Unlike most vitamins, your body can make vitamin D on its own: when your skin is exposed to ultraviolet B (UVB) rays from sunlight, it triggers vitamin D synthesis. This is why it is called the “sunshine vitamin”. However, sunlight alone often is not enough, especially if you live in a northern climate or spend most of your time indoors.
There are two main forms of vitamin D:
- Vitamin D2 (ergocalciferol): Found in some plants, fungi, and yeasts. D2 is the form often used to fortify foods and is suitable for vegetarians.
- Vitamin D3 (cholecalciferol): The form produced in human skin and found in animal-based foods. D3 is the type most vitamin D supplements contain.
So, what is the difference between vitamin D and D3? Essentially, vitamin D3 is a form of vitamin D. Studies suggest that D3 may be more effective at raising vitamin D levels in our blood than D2. In other words, if you see a supplement labeled “vitamin D3”, it is vitamin D – just the preferred form for optimal absorption.
Once vitamin D is made in your skin or ingested from food, your body must activate it through a two-step process. First, your liver converts vitamin D into a storage form called 25-hydroxyvitamin D (25(OH)D). This is the form that doctors measure in blood tests to assess your vitamin D status. Then your kidneys (and some other tissues) convert that into 1,25-dihydroxyvitamin D (calcitriol), the active hormone form that carries out vitamin D’s functions in the body. If you come across a lab report or medical note mentioning “25-hydroxy vitamin D” or “25(OH)D”, it is referring to that intermediate form – essentially the amount of vitamin D circulating in your blood.
One key thing to know is that vitamin D is fat-soluble, not water-soluble. This means any excess can be stored in body fat and is not quickly excreted in urine like vitamin C or B vitamins. Being fat-soluble is a double-edged sword: it helps you build up reserves (useful for getting through sunless winter months), but it also means taking extremely high doses could lead to a harmful buildup. We will talk more about safe dosage and toxicity later.
Key benefits of vitamin D
Vitamin D’s most famous role is in bone health. It helps your body absorb calcium and phosphate from food, which are critical minerals for building and maintaining strong bones and teeth. Adequate vitamin D, together with calcium, prevents rickets in children (a condition where bones become soft and deformed) and osteomalacia in adults (soft, fragile bones). In older adults, getting enough vitamin D can help stave off osteoporosis, a disease of thinning bones that increases fracture risk. In short, vitamin D ensures calcium from your diet goes into your bones where it belongs, rather than remaining too low or depositing in the wrong places.
Beyond bones, vitamin D has a range of other benefits and functions:
- Muscle function: Vitamin D supports muscle strength and performance. Severe deficiency can lead to muscle weakness or aches.
- Immune support: This vitamin plays a role in our immune system’s function and inflammation regulation. Research suggests that people low in vitamin D might be more prone to infections like colds and flu, and that sufficient levels help our immune cells respond effectively. (During the COVID-19 pandemic, vitamin D gained attention for potential protective effects, though more research is needed.)
- Mood and mental health: Many people refer to a better mood on sunny days – and indeed, vitamin D and mental health are connected. Low vitamin D levels have been linked with a greater risk of depression and seasonal mood changes. While taking vitamin D is not a guaranteed antidepressant, some studies find that correcting a deficiency may improve mood in those who are low.
- Chronic disease prevention: Vitamin D’s influence on cells is far-reaching. It has been studied for links to heart health, blood sugar regulation, and even cancer risk. For example, some observational studies have noted associations between low vitamin D and higher rates of type 2 diabetes, multiple sclerosis, or certain cancers. However, it is important to note that research is ongoing, and vitamin D is not a cure-all. Ensuring you have adequate vitamin D is one factor in maintaining health, but it works best alongside an overall healthy lifestyle.
- Inflammation reduction: Vitamin D can help modulate inflammation in the body. This might be one reason it is being studied in conditions like autoimmune diseases or arthritis.
In summary, why is vitamin D important? Because it touches so many aspects of our well-being – from the strength of our skeleton to the effectiveness of our immune defences. It’s one of those nutrients that has body-wide effects, which is why being deficient can make you feel generally unwell or “out of sorts” in varied ways.
Signs and symptoms of vitamin D deficiency
Vitamin D deficiency is extremely common around the world – it has been called a global epidemic. Lack of sunlight, indoor lifestyles, and limited dietary sources all contribute. But how do you know if your vitamin D is low? Here are some common signs and symptoms of a vitamin D deficiency:
- Frequent illness or infections: One of the noticeable signs can be getting sick often (for example, catching colds back-to-back). Vitamin D supports immunity, so low levels may manifest as frequent respiratory infections or slow recovery from bugs.
- Fatigue and low energy: Persistent tiredness that does not seem to have an obvious cause can be a symptom of low vitamin D. Many people with deficiency report feeling chronically fatigued or sluggish. (So if you’re wondering “will vitamin D give you energy?”, the answer is that correcting a deficiency can improve energy and reduce fatigue, but taking excess vitamin D will not act like a stimulant if your levels are already okay.)
- Muscle aches or weakness: Vitamin D is essential for muscle function, so low levels may cause muscle pain, cramps, or a general feeling of weakness in your limbs.
- Bone and joint pain: Because of its role in bone health, a lack of vitamin D can cause dull aching in your bones or lower back. In severe cases, it leads to osteomalacia, which can be quite painful in the bones and joints.
- Low mood or depression: As mentioned, some studies have linked vitamin D deficiency with depression and mood changes. You might feel more down or irritable when your vitamin D is very low.
- Hair loss and slow wound healing: These are less common, but some individuals with low vitamin D have reported hair thinning or slow healing of cuts and wounds. This is thought to be due to vitamin D’s role in skin and follicle health, as well as immune function.
In children, a severe lack of vitamin D causes rickets, which shows up as bone deformities (like bowed legs), poor growth, and developmental delays. Thankfully, rickets is preventable with adequate vitamin D. In adults, long-term deficiency can lead to osteomalacia, with symptoms of bone pain, tenderness, and weakness when walking.
It is worth noting that vitamin D deficiency symptoms can be subtle and easily mistaken for other conditions. Many people will not realize they are deficient until they have a blood test. Doctors typically define deficiency as a blood level of 25-hydroxyvitamin D below about 20 ng/mL (50 nmol/L). Levels between 20–30 ng/mL might be considered “insufficient” – not outright deficient but not optimal either. For most people, a target of at least 30 ng/mL (75 nmol/L) is considered a good level for overall health, though official recommendations vary slightly.
Who is at risk of vitamin D deficiency? You might be more prone to low vitamin D if any of the following apply to you:
- Limited sun exposure: If you spend most of your time indoors, work night shifts, or live in a northern country with weak winter sunlight (think the UK, Northern Europe, Canada, etc.), you may not get enough UVB for vitamin D. For example, in the UK from October to March, the sun is not strong enough for your skin to make vitamin D. Nordic countries experience a “vitamin D winter” where virtually no vitamin D can be produced from the sun for months. Even in very sunny regions like the Middle East, people who stay inside air-conditioned environments or wear clothing that covers most of the skin often have surprisingly high deficiency rates. In fact, despite abundant sunshine, Middle Eastern countries report widespread vitamin D deficiency, especially among women who cover up for cultural or religious reasons.
- Darker skin tone: Melanin, the pigment in darker skin, reduces the skin’s ability to produce vitamin D from sunlight. This means people with dark skin (for example, those of African, Afro-Caribbean, or South Asian heritage) need more sun exposure to make the same amount of vitamin D as someone with lighter skin. In high latitude countries, individuals with dark skin are at particularly high risk of deficiency and are often advised to take supplements year-round.
- Older age: As we age, our skin becomes less efficient at synthesizing vitamin D. Older adults are also more likely to stay indoors or have diets lacking in vitamin D. Plus, the kidneys (which activate vitamin D) may become less effective. All of this means the elderly often need vitamin D supplements to maintain adequate levels.
- Infants and young children: Babies who are exclusively breastfed are at risk of low vitamin D because breast milk contains very little of it. Young children also may not get enough sun. Without supplements, they could develop rickets. We’ll discuss specific recommendations for infants in a later section.
- Pregnant women: Pregnancy increases the body’s demand for vitamin D, and deficiency can affect both mother and baby. Many antenatal care guidelines urge pregnant women to ensure sufficient vitamin D to support the baby’s bone development and the mother’s health.
- People with certain medical conditions: Conditions that affect fat absorption (like Crohn’s disease, celiac disease, or cystic fibrosis) can lead to deficiency, since vitamin D from food needs fat to be absorbed. Additionally, kidney or liver disorders can impair the conversion of vitamin D to its active form.
- Strict vegans or those on plant-based diets: Since most natural food sources of vitamin D are animal-based, vegans may struggle to get enough from diet alone (unless they consume fortified foods or specific mushrooms). However, vegan vitamin D3 supplements derived from lichen are now available to fill this gap.
If you suspect you have vitamin D deficiency symptoms, it is wise to get a blood test through your GP or healthcare provider. The good news is that treatment for vitamin D deficiency is usually straightforward: it involves taking supplements (often high-dose ones for a short period if you’re very deficient) and then maintaining with daily moderate doses. In severe cases or if absorption is a problem, a doctor might prescribe a vitamin D injection or a concentrated oral dose (sometimes known as a “Stoss therapy”) to quickly boost levels. These approaches are typically under medical supervision.
(On a technical note, if you ever see “Vitamin D deficiency – ICD-10 E55” in your medical records, that is just the coding used by doctors and insurers to classify the diagnosis.)
Top food sources of vitamin D
Vitamin D is famously tricky to get from food – there are not many foods that naturally contain vitamin D. That is why many countries resort to fortifying certain foods and why supplements are so common. However, here are some of the best food sources of vitamin D to include in your diet:
- Oily fish: Fatty fish are by far the richest natural source. Salmon, mackerel, sardines, herring, trout, and tuna all provide a good dose of vitamin D. For example, a portion of salmon can easily give you more than the daily requirement of vitamin D (especially wild salmon, which tends to have more than farmed). Cod liver oil – while technically a supplement rather than a food – is an old-school source extremely high in vitamin D (just a teaspoon of cod liver oil contains a whopping amount of vitamin D, along with vitamin A). If you go this route, be cautious not to overdo it, as cod liver oil in large amounts could lead to too much vitamin A.
- Egg yolks: Eggs contain some vitamin D, mostly in the yolk. The amount can vary – eggs from chickens given vitamin-D-enriched feed or that roam outdoors (pasture-raised hens) will have more vitamin D in their yolks. While an egg will not supply all your daily vitamin D, it can contribute.
- Red meat and liver: Meat is not a huge source, but there is a small amount of vitamin D in red meat. Liver (such as beef liver) contains vitamin D as well. However, pregnant women should avoid eating liver frequently because it’s very high in vitamin A, which can be harmful to the baby in large quantities.
- Milk and dairy (fortified in some countries): In many countries like the United States and Canada, cow’s milk is fortified with vitamin D, meaning the dairy producers add vitamin D to milk to help the population meet requirements. A glass of fortified milk typically provides around 100 IU (2.5 µg) or more. Some yogurts and cheeses may also be fortified, but typically not to the same extent. Important for UK readers: In the UK, milk is generally not fortified with vitamin D (with the exception of some special products). So, unlike in the US, drinking milk in Britain will not give you a vitamin D boost unless the label specifically says it is added.
- Margarine and spreads: Several countries mandate fortification of margarines or fat spreads with vitamin D (and vitamin A) to mimic the nutrients found in butter. For instance, in the UK some fat spreads and margarines have vitamin D added. Always check the packaging.
- Breakfast cereals and other fortified foods: Many breakfast cereals, orange juices, plant-based milk alternatives (soy milk, almond milk, oat milk, etc.), and even some breads are fortified with vitamin D. These can be valuable sources especially for vegetarians or vegans. The levels added vary by product, so again, labels are your friend. Combining a few fortified foods (like cereal + fortified plant milk) can add up.
- Mushrooms: Most fruits and vegetables will not give you vitamin D, but mushrooms are the exception – and even then, only if treated properly. When mushrooms are exposed to UV light (either sunlight or special lamps), they can produce vitamin D2, similar to how our skin makes D3. Some wild mushrooms like chanterelles or morels naturally have vitamin D if they have had sun exposure. Today, you can even find certain mushroom products (fresh or powdered) that have been UV-exposed and are marketed as high in vitamin D. For a plant-based diet, UV-exposed mushrooms are a useful addition. However, standard white button or portobello mushrooms grown in the dark have negligible vitamin D unless the package states they are UV-treated. Keep in mind, mushroom-derived D2 may be slightly less bioactive than D3, but it is still beneficial.
In general, foods rich in vitamin D are relatively few, and one has to make a deliberate effort to include them. Oily fish is the standout source. For vegetarians, dairy and eggs can help if they are fortified or the hens had sunlight exposure. For vegans, apart from UV-exposed mushrooms, it really comes down to fortified foods (and supplements).
If you are wondering “what foods are high in vitamin D?” or “which foods are the best source of vitamin D?”, the answer is clear: oily fish wins, with fortified foods playing a major supporting role. You might also ask, “are there fruits with vitamin D or vitamin D in vegetables?” The truth is, naturally, fruits and most veggies do not contain vitamin D. A pineapple or a carrot won’t boost your D levels. This is why even a “healthy diet” might still leave you vitamin D deficient if you rely solely on plants and do not get sunlight – you’d need to incorporate fortified foods or take a supplement.
Getting vitamin D from the sun: Of course, diet is not the only way. Sun exposure on bare skin (without sunscreen, for a short period) can produce significant vitamin D in the summer months. Just 10-15 minutes of midday sun on arms and face a few times a week can be enough for lighter-skinned individuals during summer. Those with darker skin may need longer exposure. The body cleverly stores vitamin D made in summer in body fat, releasing it during winter to some extent. However, relying on sun alone is tricky: factors like latitude, season, time of day, weather, pollution, and use of sunscreen all determine how much vitamin D you can make. Always balance sun exposure with skin cancer risk – never stay out so long that you burn. Short, regular bouts of sunshine are best. If you have very limited sun (such as long dark winters or you must avoid sun for health reasons), then food and supplements become your main sources.
Vitamin D supplements and how to take them
Given how challenging it can be to obtain enough vitamin D from food and sun alone, vitamin D supplements are extremely popular and often recommended. Here is what you should know about supplements, including the different forms and the best way to take them:
Forms of vitamin D supplements:
- The majority of supplements contain vitamin D3 (cholecalciferol), because it is the same form your body makes from sun and is very effective at raising blood levels. Traditional D3 supplements are typically sourced from lanolin (the oil in sheep’s wool), but vegan D3 made from lichen is also available if you prefer to avoid animal products.
- Some supplements (and prescription high-dose pills) use vitamin D2 (ergocalciferol). D2 is the plant-based form. It can still treat or prevent deficiency, but you might need slightly higher doses of D2 to achieve the same effect as D3. In general, unless you are vegan, D3 is the go-to choice.
- Vitamin D supplements come in various formats: the most common are tablets or capsules, including softgels. There are also vitamin D drops (liquid form) which are useful for infants and children or anyone who has trouble swallowing pills. Just a drop or two can deliver the required dose for a baby – these are often called vitamin D infant drops or “D drops”. Chewable gummies are another option that both kids and adults sometimes prefer (vitamin D gummies often taste like fruit candy, but be mindful of added sugars). Additionally, some brands offer vitamin D as an oral spray that you spritz in your mouth.
- For individuals with severe deficiency or certain medical conditions, doctors might administer vitamin D injections (also known as vitamin D shots). This is not routine for most people, but it can rapidly correct a dangerously low vitamin D level or bypass absorption problems in the gut. An injection typically contains a mega-dose (like 300,000 IU) that releases slowly. Again, this is only done under medical supervision.
Combining vitamin D with other nutrients: You will notice some supplements pair vitamin D with other vitamins or minerals. Common combos include vitamin D and calcium (often in bone health formulas), vitamin D and K2, or vitamin D with magnesium. These combinations exist for good reason:
- Vitamin D and calcium: This duo is classic for bone health. Many studies have used combined calcium and vitamin D supplements to reduce fracture risk in older adults. If you take a calcium supplement, having some vitamin D with it helps ensure the calcium will be absorbed and used. (However, consult your doctor about taking calcium supplements; some people get enough calcium from diet and don’t need a pill, and excessive calcium supplementation has been linked to kidney stones and other issues in some cases.)
- Vitamin D and vitamin K2: Vitamin K2 (a form of vitamin K) works synergistically with vitamin D in bone metabolism. It helps guide calcium into bones and teeth and may help prevent calcium from depositing in arteries. There is a lot of buzz about this combo recently. Some early research indicates that taking vitamins D and K together could modestly improve bone density and reduce arterial calcification compared to taking D alone. While we do not have conclusive evidence that everyone needs to take K2 with D, combination D3+K2 supplements are popular and generally considered safe. If your diet is low in K (found in leafy greens and fermented foods), a bit of K2 with D might be beneficial. As always, discuss with a healthcare provider if you have any conditions or are on blood-thinning medication (since vitamin K affects blood clotting).
- Vitamin D and magnesium: Magnesium is another unsung hero in the vitamin D story. Your body needs magnesium to convert vitamin D into its active form. If you are low in magnesium, vitamin D supplementation might not work as effectively, and you could also be more prone to side effects like cramps. In fact, magnesium and vitamin D have a cooperative relationship: vitamin D helps you absorb magnesium, and magnesium helps activate vitamin D. Many people are a bit low in magnesium (found in nuts, seeds, greens, whole grains), so some experts recommend ensuring magnesium intake is adequate when taking vitamin D. You can achieve this through diet or with a magnesium supplement if needed. It is generally safe to take magnesium and vitamin D together – some people even find taking magnesium in the evening along with vitamin D can aid sleep and prevent any nighttime restlessness. The key is not to exceed safe limits for magnesium supplements (typically no more than 350 mg of supplemental magnesium per day for adults, unless directed by a doctor, as too much magnesium can cause diarrhea).
When and how to take vitamin D: A common question is “what is the best time to take vitamin D?” The truth is, vitamin D can be taken at any time of day, but there are a couple of tips to maximize its effectiveness:
- Take it with food: Because vitamin D is fat-soluble, it is best absorbed when you have it alongside some fat. Taking your D pill with a meal or snack that contains a bit of healthy fat (like olive oil, avocado, nuts, eggs, etc.) can boost absorption. If you take it on an empty stomach, you might absorb less of it.
- Morning vs. evening: There is not a hard rule here, but some people prefer taking vitamin D earlier in the day. There is anecdotal talk that taking vitamin D late at night might interfere with sleep in some individuals (possibly because it might have a mild energizing effect for those who were deficient). While scientific evidence on the timing is not conclusive, if you find you sleep better when taking it in the morning, go for it. Otherwise, taking it in the evening with dinner is perfectly fine for most. The priority is consistency – take it at a time you’ll remember each day.
- Consistency matters: Vitamin D is not a supplement you feel immediately (it is not like a painkiller or caffeine). It works in the background, maintaining your bones and immune function. The benefits come with regular use over time. So, whichever time of day you choose, make it a habit. Some people set a reminder or keep the bottle by their toothbrush or kettle as a cue.
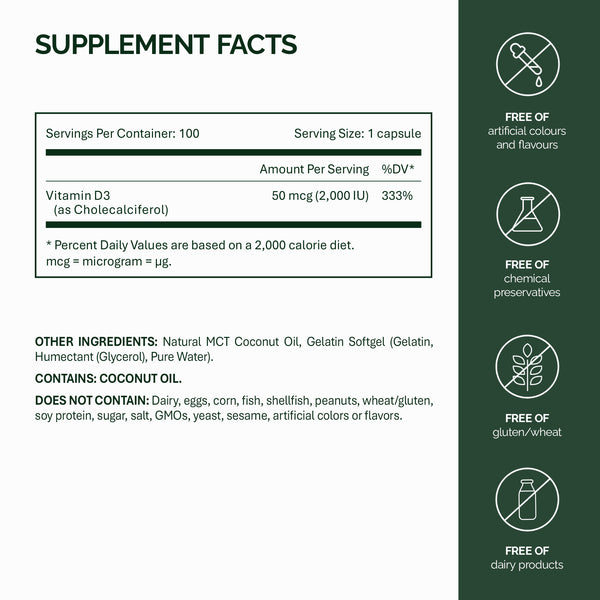
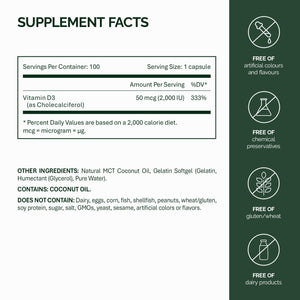
Choosing a supplement and dosage: Vitamin D supplements are available in various strengths. Common doses include 400 IU (10 µg), 1,000 IU (25 µg), 2,000 IU (50 µg), and 4,000 IU (100 µg) per pill/drop. There are also higher doses like 10,000 IU, but those are generally for short-term use under medical advice.
For general health maintenance, many adults in the UK are advised to take 10 micrograms (400 IU) of vitamin D daily during autumn and winter. In fact, the UK government (as well as health authorities in several countries) recommends that everyone over 4 years old should consider taking 10 µg daily throughout winter, and year-round if you have limited sun exposure. In the summer months, if you are regularly outdoors, you might not need a supplement as your body can make enough. However, it will not hurt most people to continue the low-dose supplement year-round, especially since typical diets do not provide much.
In the USA and many other countries, the recommended dietary allowance is around 600 IU (15 µg) per day for adults and 800 IU (20 µg) for older adults. These amounts are considered sufficient for bone health in the general population. Some experts and professional societies suggest higher intakes (like 1,000–2,000 IU daily) for certain individuals or to optimize levels around 30 ng/mL, but opinions vary. The consensus is that at least 400–800 IU daily is needed for most people to avoid deficiency, and higher doses may be needed for those with known low levels or risk factors.
Let’s look at specific groups and their needs:
- Infants (0-12 months): Babies have very sensitive skin and should not be exposed to strong sun, so they often need a supplement. In the UK, it is recommended that all babies from birth to one year who are breastfed (or having less than 500ml of formula a day) are given 8.5 to 10 µg of vitamin D daily. Infant formula is usually fortified with vitamin D, so babies on more than 500ml of formula typically get enough from that, but exclusively breastfed babies do need the drops. These are often called vitamin D drops for infants or “D drops”. They are easy to administer – you can put the drop on the nipple, a clean finger, or mix into a little milk. Ensuring infants have enough vitamin D prevents rickets and supports healthy growth.
- Young children (1-4 years): Toddlers and preschoolers are also advised to take 10 µg (400 IU) vitamin D daily. This is because at these ages, diets might still be limited and their growing bones need support. Plus, we cannot rely on them getting lots of sun, especially if they’re mostly indoors or well-covered when outside. Children’s vitamin D drops or chewy vitamins can be used. In the UK, families on certain benefits can get free vitamin D drops for kids under the Healthy Start scheme.
- Pregnant and breastfeeding women: Pregnancy increases the need for vitamin D slightly, but health guidelines usually keep it simple: pregnant women should take the same 10 µg (400 IU) daily that is recommended for other adults. This ensures both mum and developing baby have enough for bone health and immune function. There is some research into whether higher vitamin D in pregnancy could reduce complications like pre-eclampsia or low birth weight, but as of now, the standard advice is 10 µg unless a deficiency is identified (in which case a doctor might prescribe more). Breastfeeding women also should continue with at least 10 µg daily. It is worth noting that breast milk is very low in vitamin D, hence the need to supplement the baby directly as mentioned above. High-dose vitamin D taken by the mother can somewhat increase levels in breast milk, but routine maternal high dosing is not generally recommended without medical supervision.
- People with little sunlight year-round: This includes certain office workers, those who are housebound or in care homes, people who wear veils or cover most of their skin for cultural reasons, and even those in extremely sunny climates who simply stay indoors (e.g. to avoid the heat) or always use heavy sunscreen. If you fall into this category, health authorities recommend taking a daily supplement of 10 µg vitamin D throughout the entire year, not just winter. For example, someone living in the Middle East who goes from home to car to office and back, without regular sun on their skin, should treat it as if they live in a sunless country – they need to get vitamin D through diet or supplements consistently. Likewise, an elderly person in a care home who rarely goes outside should be supplemented daily.
- Northern latitude residents (Nordic countries, etc.): If you live far north, you might consider higher vitamin D intake or strict supplement adherence, because the winter is long and even summer sun angles might be mild. Interestingly, countries like Finland and Sweden have implemented robust food fortification policies (adding vitamin D to milk, spreads, etc.) to help their populations maintain better vitamin D status. So, check if foods in your country are fortified. If not, definitely keep up with a supplement especially from autumn through spring.
- Vegans and vegetarians: As noted earlier, plant sources of vitamin D are scarce. If you do not consume fish, eggs, or dairy, you should be diligent about vitamin D. Look for fortified plant milks, cereals, and consider a supplement. Many multivitamins or specific vegan vitamin D supplements will cover this. Thankfully, vegan D3 (from lichen) is now common, so you do not have to settle for D2 only.
- People trying to lose weight: This might sound like an odd category, but there’s some evidence that vitamin D can get “trapped” in fat tissue. Overweight and obese individuals often have lower bioavailable vitamin D. They might need a higher dose to maintain the same blood level as a lean person. If you are on a weight loss journey, also ensure you are replete with vitamin D – not because vitamin D will cause weight loss, but because it is supporting your overall health while you shed fat (and potentially release stored vitamin D back into circulation). Some doctors will give higher daily doses or monitor levels in overweight patients.
Dosage guidelines and safety (avoidance of deficiency and toxicity)
We have touched on some dosage points above, but let us summarise how much vitamin D is ideal and how to avoid taking too little or too much:
- General daily recommendations: For most adults, 10–20 micrograms per day (400–800 IU) is a solid intake range that prevents deficiency. In practice, many supplements come as 25 µg (1000 IU), which is fine for everyday use. Taking 1000 IU daily will ensure most people reach a blood level in the sufficient range. If you get a lot of sun in the summer, you might opt for the lower end (400 IU) in winter. If you have darker skin or other risk factors, you might lean towards the higher end (800–1000 IU). Remember, these moderate doses are preventive and meant to maintain good health.
- If you are deficient: If a blood test shows you are vitamin D deficient, doctors often prescribe higher doses temporarily. Common protocols might be 20,000 IU once a week, or 4,000 IU daily, or even 50,000 IU once a week for a few weeks, to quickly build up levels. These are short-term therapeutic doses. Always follow your healthcare provider’s instructions in these cases – more is not better unless monitored. After replenishment, you will typically go back to a maintenance dose.
- Safe upper limits: Taking too much vitamin D can be harmful, so it is crucial to know the upper safe limit. For adults (including pregnant or breastfeeding women) and children over 11, the upper limit is about 100 µg per day – that is 4,000 IU daily. Exceeding 4,000 IU regularly is not advised unless under medical advice. Children 1-10 years should not exceed 50 µg (2,000 IU) daily, and infants under 12 months should stay below 25 µg (1,000 IU) daily. These limits include all sources (food+supplements). To put it into perspective, you would generally have to take a lot of high-dose pills to reach these levels – it is unlikely to overdose from typical over-the-counter doses like 1,000 or 2,000 IU. But problems have arisen when people megadose erroneously (for instance, taking tens of thousands of IU daily for months, which is unnecessary and risky).
- Vitamin D toxicity: Having “too much of a good thing” definitely applies to vitamin D. Vitamin D toxicity (hypervitaminosis D) is rare but serious. It leads to hypercalcemia, a condition where calcium levels in the blood become too high. Hypercalcemia can cause a range of unpleasant symptoms: nausea, vomiting, loss of appetite, abdominal pain, constipation, excessive thirst and urination, weakness, confusion, and kidney stones. In severe cases, it can even cause kidney damage or heart rhythm disturbances. Essentially, too much vitamin D forces too much calcium into the bloodstream. If you’ve ever heard someone ask “can vitamin D cause constipation?” – this is where that comes from. Vitamin D itself at normal doses doesn’t cause constipation, but vitamin D toxicity leading to hypercalcemia can cause constipation as one of its symptoms. The threshold for toxicity is not set in stone, but generally regularly taking more than 10,000 IU/day for an extended period could put you at risk, and some cases have occurred from doses as low as 5,000 IU/day in susceptible individuals. The good news is you cannot overdose on vitamin D from sun exposure – your skin has a self-regulating mechanism and will stop producing D when you have had enough sun, plus some vitamin D is degraded in the skin after lots of sun. So, vitamin D toxicity only happens from supplements (or occasionally from industrial accidents where food is over-fortified).
- Signs of too much vitamin D: If you are taking high-dose supplements and start feeling unwell with the symptoms mentioned (persistent nausea, severe lack of appetite, frequent vomiting, very thirsty and peeing a lot, constipation, confusion), it could be a red flag of excess vitamin D/hypercalcemia. Stop the supplements and see a doctor for a calcium level check. Treatment usually involves stopping vitamin D and reducing calcium until levels normalize. Again, this is rare – the vast majority of people will never experience vitamin D toxicity, especially if sticking to recommended doses.
- Interactions and precautions: Vitamin D can interact with certain medications. For instance, if you are on certain cholesterol-lowering drugs (statins) or tuberculosis medication (rifampicin) or anti-seizure meds, these can increase the breakdown of vitamin D, meaning you might need more. Conversely, taking high doses of vitamin D can reduce the effectiveness of statins. Also, if you are on a diuretic (thiazide diuretic) for blood pressure, high vitamin D intake could cause your blood calcium to rise too much. If you take oral steroids long-term, they can lower vitamin D levels. And notably, if you are on warfarin (a blood thinner), high doses of vitamin K supplements can interfere with it – so if you start a combo vitamin D+K supplement, inform your doctor. These are specific situations; generally vitamin D is very safe, but always check with a pharmacist or doctor if you are starting a supplement and you have underlying health conditions or medications.
To sum up the safety aspect: vitamin D is crucial, but balance is key. Ensure you get enough to stay out of deficiency, but do not go to extremes thinking megadoses will make you superhuman. More is not necessarily better and can be harmful. For most folks, a moderate daily supplement, attention to diet, and a bit of sunshine will do the trick.
Conclusion
Vitamin D may be a single nutrient, but its impact on our health is far-reaching. To recap:
- Benefits: It strengthens bones and teeth by helping calcium do its job, supports muscle function, bolsters the immune system, and likely influences mood and long-term wellness. It is a foundation for a healthy body, explaining why we feel off-kilter when we are low.
- Sources: Our bodies can make vitamin D from sun exposure – but modern life and geography do not always allow enough sun. Fatty fish, egg yolks, liver, and UV-exposed mushrooms are among the few natural food sources. Many countries fortify foods like milk, cereals, and margarines with vitamin D to help out. Still, diet alone often is not sufficient for optimal levels.
- Deficiency: Vitamin D deficiency is common and can creep up on you, with subtle signs like fatigue, frequent colds, or low mood. In more severe cases, it affects bone health (rickets in kids, soft bones in adults). Certain groups – including infants, young children, pregnant women, the elderly, people with dark skin in low-sun climates, and anyone who avoids sun – should be particularly vigilant and consider supplements.
- Supplements: Vitamin D supplements (usually D3 form) are a safe and effective way to ensure you meet your needs, especially in winter. A daily dose of around 10–20 µg (400–800 IU) is recommended for most adults, with specific dosing for babies and children as advised. Take it with a meal for best absorption, and stay consistent.
- Safety: Vitamin D is fat-soluble, so it can accumulate. Stick to recommended doses (no more than 100 µg or 4,000 IU daily for adults, unless directed by a doctor). That gives you a large safety margin. Avoid mega-dosing on a whim – more is not automatically more beneficial and could lead to toxicity over time, which brings its own set of problems. You cannot overdose from sunshine, so enjoy the sun wisely for a natural top-up, but use supplements responsibly.
In a gloomy northern winter or for those who rarely see the sun, a simple vitamin D pill can be a game-changer for health and well-being. Conversely, if you are fortunate to have plenty of sun year-round, remember to still balance sun safety with your body’s needs – moderate sun exposure can be very helpful, but supplements are a zero-UV risk alternative.
Bottom line: Vitamin D is essential for everyone, from newborns to the elderly. It is one vitamin where a little planning goes a long way – a bit of sunshine here, a glass of fortified milk or a piece of salmon there, or a daily supplement when needed, and you’ll reap the benefits of this powerhouse nutrient. Make vitamin D your ally, and your body will thank you with stronger bones, a more robust immune system, and better overall vitality. Stay healthy, and let the “sunshine vitamin” brighten your days (even when the sun is nowhere to be seen)!
References
- Office of Dietary Supplements, National Institutes of Health – Vitamin D Fact Sheet for Health Professionals ods.od.nih.govods.od.nih.gov
- NHS (UK) – Vitamin D (Benefits, Sources, Dosage, Deficiency) nhs.uknhs.uk
- Healthline – Wartenberg & Spritzler (2024) Common Symptoms of Vitamin D Deficiency and How to Treat Them healthline.comhealthline.com
- Scientific Reports (AlFaris et al., 2019) – Vitamin D Deficiency in Middle East Women (Riyadh study) nature.com
- Health.com – Benefits of Taking Vitamin D and K Together health.comhealth.com
- Drugs.com – Hannemann (2025) Q&A: Magnesium with Vitamin D drugs.comdrugs.com
- Cleveland Clinic – Vitamin D Toxicity (Hypervitaminosis D) Overview my.clevelandclinic.org
- NIH Office of Dietary Supplements – Vitamin D: Recommended Intakes & Sources ods.od.nih.gov
- NHS – Vitamin D: Advice for at-risk groups and infants nhs.uknhs.uk
- Health.com – Vitamin D2 vs D3 Absorption health.com