What is TUDCA?
TUDCA (tauroursodeoxycholic acid) is a water-soluble bile acid that our bodies naturally produce. It is formed when gut bacteria convert primary bile salts into ursodeoxycholic acid (UDCA), which then bonds with the amino acid taurine. In medicine, TUDCA (like UDCA) is used to treat cholestasis – a condition where bile fails to flow normally – and can help dissolve cholesterol gallstones.
In plain terms, TUDCA is a bile component that aids fat digestion and protects liver cells.
How does TUDCA work?
TUDCA acts as a cellular “chemical chaperone,” helping proteins fold correctly and reducing stress in the endoplasmic reticulum (ER). By lowering ER stress, cells (especially in liver and muscle) function more efficiently. For example, in obese mice, TUDCA treatment reduced ER stress, improved insulin resistance, and even decreased liver fat. In effect, TUDCA supports overall cellular health and metabolism by helping cells handle excess proteins or fats without damage.
Potential Benefits of TUDCA
-
Liver & Gallbladder Health: TUDCA promotes healthy bile flow and protects liver cells. It’s used clinically for cholestasis and fatty liver. In trials, TUDCA dramatically lowered liver inflammation markers (ALT, AST, ALP) and improved liver function in conditions like cirrhosis, hepatitis, and cholestasis. It also safely helps dissolve cholesterol gallstones into smaller fragments that can pass through the bile ducts.
-
Metabolic Support: TUDCA can improve insulin sensitivity and blood lipid profiles. In one human study, obese individuals given ~1,750 mg/day of TUDCA experienced about 30% improvement in liver and muscle insulin sensitivity. TUDCA has also been shown to lower total cholesterol (and raise HDL). Together, these effects suggest TUDCA helps regulate blood sugar and supports healthy cholesterol levels.
-
Cellular Stress Reduction: By acting as a chaperone, TUDCA helps cells manage excess proteins and fats without triggering inflammation. This cell-protective effect supports mitochondria (our cells’ energy centers) and other organelles, promoting healthier cell function overall. In short, TUDCA can act like a “detox helper” at the cellular level.
-
Neuroprotection (Preclinical): In laboratory studies, TUDCA shows promise for protecting brain and retinal cells. It prevented cell death in animal models of Alzheimer’s, Parkinson’s, ALS, and retinal degeneration. These findings are preclinical only (i.e. in animals or cell cultures), but they point to TUDCA’s potential to protect stressed neurons and retinal cells. More human research is needed, but the early data is encouraging.
-
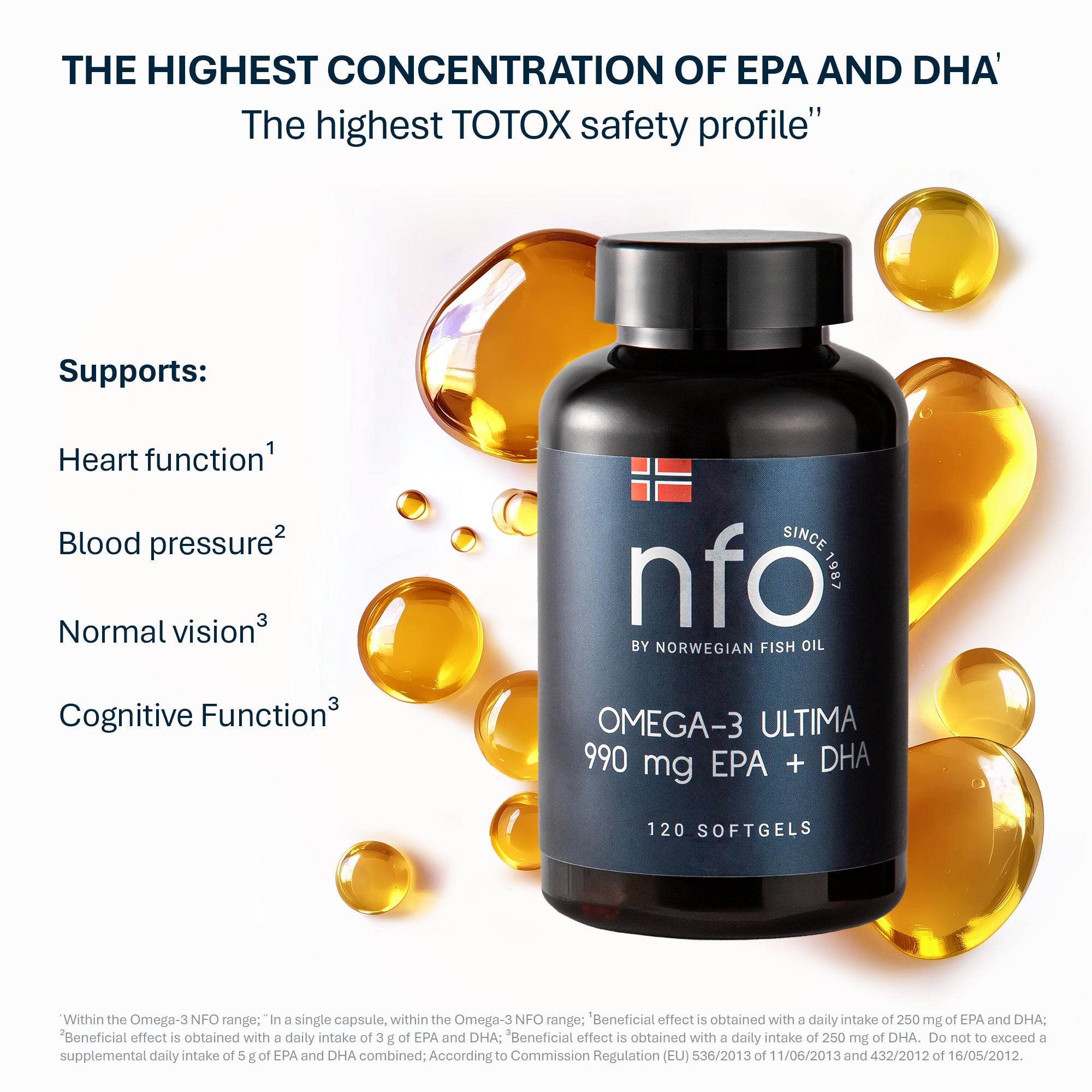
Omega-3 Synergy: Interestingly, TUDCA and omega-3 fatty acids appear to complement each other. One study found that TUDCA partially restored omega-3 levels in the liver under stress and actually supports the use of omega-3 supplements for liver health. Separately, clinical research shows that EPA/DHA omega-3 supplements safely lower liver fat and inflammation in fatty liver disease. Taken together, TUDCA (which aids bile flow and cell health) and omega-3s (anti-inflammatory fats) can work hand-in-hand to protect the liver and metabolism.
TUDCA and Omega-3: working together
Both TUDCA and omega-3 supplements have anti-inflammatory, liver-supporting effects. TUDCA helps preserve omega-3 fatty acids in the liver under stress, while omega-3s from fish oil are well-known to reduce liver fat and oxidative damage. In practice, taking TUDCA alongside an omega-3 supplement (EPA/DHA) may provide extra benefits: studies suggest the combination could improve blood lipids and protect liver cells more effectively than either alone.
Safety and dosage
TUDCA is generally well-tolerated in adults. Human and clinical data report few side effects. For example, an observational study in ALS patients found only about 8% of subjects stopped taking TUDCA due to mild gastrointestinal discomfort (nausea or diarrhea). Even at high doses, TUDCA was described as "generally safe and well-tolerated". That said, like any supplement, it can cause stomach upset in some people (especially at first or at high doses), so it's wise to start with a low dose and take it with food.
What about dosage? Studies have used a wide range. Some trials found benefits with very low doses (as little as 10–13 mg/day for liver regeneration), while others went up to 1,750 mg/day. Most TUDCA supplements recommend 250–1,000 mg per day (often split into 2 doses). Since research is still evolving, there is no single “correct” dose for everyone. Always consult your doctor before starting TUDCA, especially if you have gallbladder disease, bile duct issues, or are on other medications.
Conclusion
In summary, TUDCA (tauroursodeoxycholic acid) is a naturally occurring bile acid with strong science behind its use for liver and metabolic health. Clinical studies show it can improve liver function, support healthy digestion of fats, enhance insulin sensitivity, and lower inflammation. It works at the cellular level to reduce ER stress, which translates to broader benefits for the liver, pancreas, and other tissues. Early research even suggests neuroprotective benefits (in lab models).
For general readers, think of TUDCA as a powerful liver-support supplement. It complements a healthy diet, exercise, and other nutrients (like omega-3s) to help keep your liver and cells healthy. Pairing TUDCA with omega-3s or other anti-inflammatory nutrients, along with sensible lifestyle habits, may maximize its benefits for your liver and overall wellness.
References
-
Beuers, U. et al. (1998). The biliary system: bile acids, bile secretion, and cholestasis. Journal of Hepatology, 28(Suppl 1), 2–8.
-
Kars, M. et al. (2010). Tauroursodeoxycholic Acid May Improve Liver and Muscle Insulin Sensitivity in Obese Men and Women. Diabetes, 59(8), 1899–1905. https://doi.org/10.2337/db10-0308
-
Han, J. et al. (2017). TUDCA reverses an ER stress–induced decrease in hepatic omega-3 fatty acid levels. Journal of Lipid Research, 58(9), 1775–1785.
-
Elia, A.E. et al. (2016). Tauroursodeoxycholic Acid in the Treatment of Patients With Amyotrophic Lateral Sclerosis. European Journal of Neurology, 23(1), 45–52.
-
Keene, C.D. et al. (2002). Tauroursodeoxycholic acid, a bile acid, is neuroprotective in a transgenic model of Huntington’s disease. PNAS, 99(16), 10671–10676.
-
Gonzalez-Polo, R.A. et al. (2005). TUDCA prevents apoptosis by inhibiting the release of cytochrome c from mitochondria. Cell Death and Differentiation, 12(8), 921–931.
-
Cao, S.S., & Kaufman, R.J. (2012). Endoplasmic Reticulum Stress and Oxidative Stress in Cell Fate Decision and Human Disease. Antioxidants & Redox Signaling, 21(3), 396–413.
-
Poupon, R. et al. (1991). Effect of UDCA and TUDCA on cholestatic liver diseases: A comparative overview. Hepatology, 13(5), 913–920.
-
Parés, A. et al. (2006). Effects of tauroursodeoxycholic acid in patients with primary biliary cirrhosis. Hepatology, 44(1), 111–117.
-
Aller, R. et al. (2008). Effect of Tauroursodeoxycholic Acid on Liver Enzymes and Liver Fat in Nonalcoholic Fatty Liver Disease Patients. European Review for Medical and Pharmacological Sciences, 12(6), 307–315.
-
Ratziu, V. et al. (2010). Omega-3 fatty acids in non-alcoholic steatohepatitis: A randomized controlled trial. Hepatology, 52(4), 1448–1457.
-
Angulo, P. et al. (2015). Liver Fibrosis, but No Other Histologic Features, Associates with Long-term Outcomes of Patients with Nonalcoholic Fatty Liver Disease. Gastroenterology, 149(2), 389–397.e10.
-
Vang, S. et al. (2014). TUDCA prevents ER stress and corrects insulin signaling defects in cells and obese mice. Diabetes, 63(7), 2468–2477.